Menopause: Misrepresented as a 'Disease' by Commercial Interests
Medical researchers in the US, UK, and Australia highlight healthier perspectives on menopause in lower-income countries.
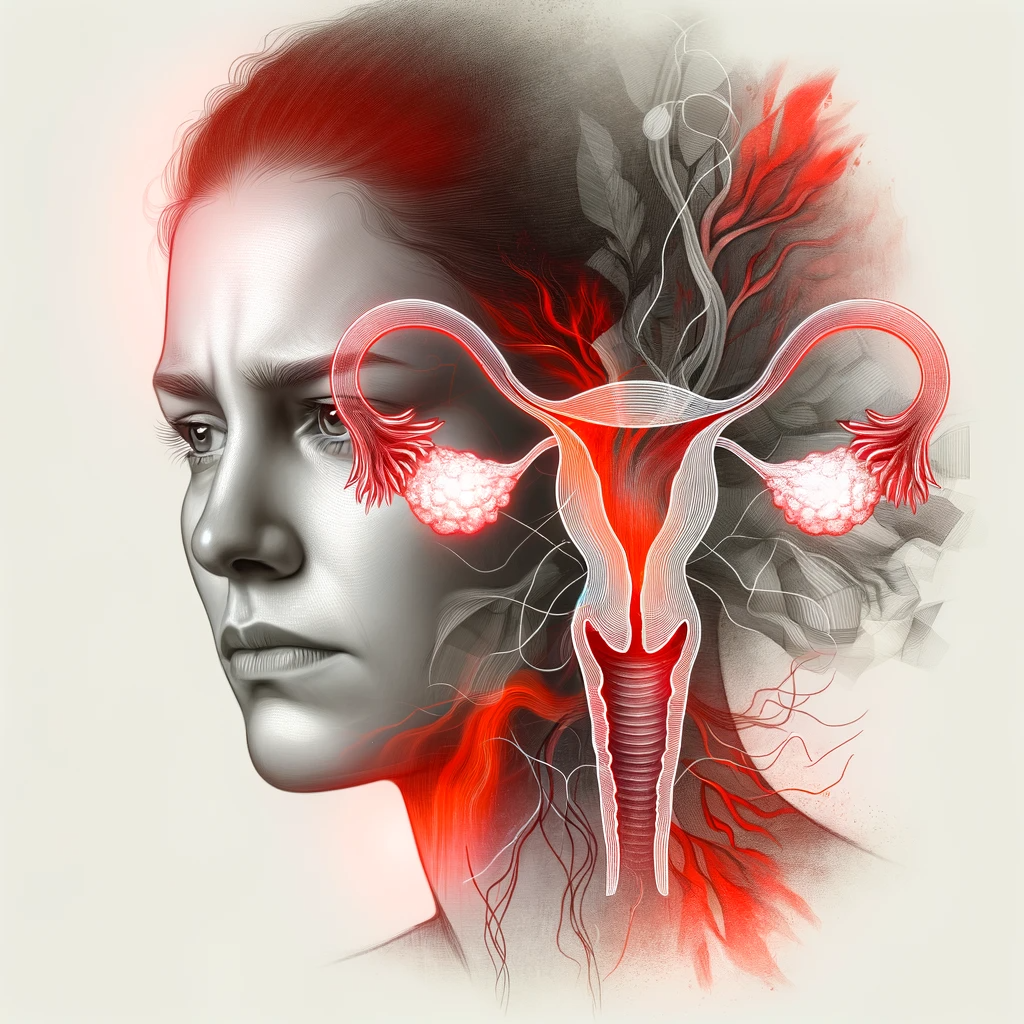
According to the US National Institute on Aging (NIA) of the NIH and the World Health Organization (WHO), menopause is not a disease or disorder; it is a natural stage of a woman's life.

However, a series of papers published in the Lancet recently reveals how drug companies profit from portraying menopause as a “disease,” leading to misinformation and ineffective treatments of hormonal drugs for women.
Overmedication with hormonal drugs to treat non-diseases has negatively impacted women's health in developed countries, leading to increased incidences of many serious diseases like breast cancer, heart attacks, and strokes.

This finding has spurred leading doctors and researchers from these countries to advocate for a societal shift challenging these misconceptions.
The review of medical literature on menopause found that misguided or harmful attitudes toward menopause were prevalent in high-income countries.
These nations should learn from societies where women's aging is respected, and menopause views are more affirming, the paper suggests. For instance, Indigenous communities in Australia view menopause as less problematic.
The focus should shift from assuming midlife depression often stems from menopause to promoting gender equity and safety throughout life, particularly since early adversity increases the risk of poor mental health during midlife.
 Lead author Prof. Martha Hickey from the University of Melbourne, along with co-authors, expressed concern over the media’s tendency to sensationalize menopause, depicting it as a distressing experience only solvable with hormone replacement therapy.
Lead author Prof. Martha Hickey from the University of Melbourne, along with co-authors, expressed concern over the media’s tendency to sensationalize menopause, depicting it as a distressing experience only solvable with hormone replacement therapy.
The paper argues that while menopausal hormone therapy (MHT) may be necessary for some, evidence shows it effectively treats only hot flashes and night sweats, not other symptoms. Moreover, there's a small but serious risk of breast cancer associated with MHT use.
The authors emphasize the importance of impartial information dissemination, given that pharmaceutical companies heavily influence messaging around menopause and hormone therapy.

Another paper introduces the first clinical tool for diagnosing and managing early menopause, affecting one in 10 women globally.
Dr. Lydia Brown from the University of Melbourne led a paper focusing on promoting good mental health during perimenopause, highlighting the importance of acknowledging individual differences in women's experiences.
Prof. Susan Davis from Monash University stresses the need for an evidence-based approach and empowerment of women during menopause.
Dr. Sarah White, CEO of Jean Hailes for Women’s Health, underscores the emergence of a for-profit industry associated with menopause, which risks overshadowing open discourse about aging and menopause.
The series concludes that there's an urgent need for greater awareness, new treatments, and additional support for individuals experiencing early menopause, menopause after cancer treatment, or a higher risk of depression during perimenopause.

Since menopause is not a disease but a natural phase of life, it does not inherently require medication. Therefore, using potent drugs like estrogen to treat this normal transition can be considered overmedication.
The World Health Organization views overmedication as a significant public health concern, contributing to millions of global hospitalizations due to adverse drug reactions and accounting for billions of dollars in unnecessary healthcare expenses.
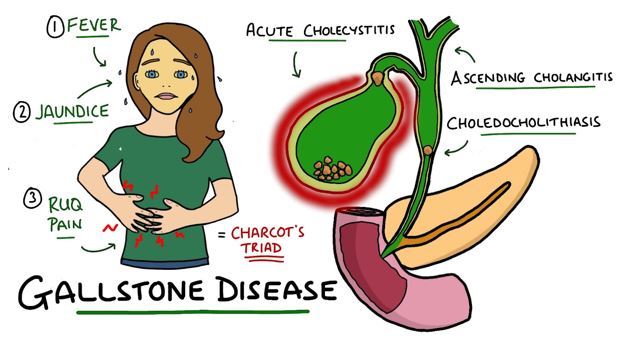
Overmedication through estrogen supplementation may provide short-term relief, but it has long-term consequences. It not only increases healthcare maintenance costs but also elevates the risk of numerous diseases, including heart disease, stroke, thrombosis, gallbladder diseases, uterine fibroids, and breast and uterine cancers.
Drug companies attempt to downplay the risk of estrogen in causing breast cancer, but recent research from scientists at Harvard has revealed that estrogen not only increases the risk of developing breast cancer but also directly contributes to its onset. This alarming discovery underscores the urgent need to explore safer and more effective alternatives to estrogen to safeguard women's health.
NeuEve offers a safer and more effective alternative to estrogen. It is not a drug but a food-grade natural product.
To date, NeuEve has helped over 100,000 women find relief safely from menopause-related vaginal dryness, including many who tried estrogen unsuccessfully and breast cancer survivors who cannot use estrogen.

NeuEve has achieved a scientific breakthrough in women's health. It effectively and safely relieves menopause-related vaginal dryness without the need for hormones.
This article explains how NeuEve works.
Disclaimer: This article is for informational purposes only. It discusses natural products, nutrients, and alternative methods for managing discomforts associated with vaginal dryness (not a true disease). It is not intended as medical advice for the treatment of any diseases.








Leave a comment